Canada's Health Care System
Introduction
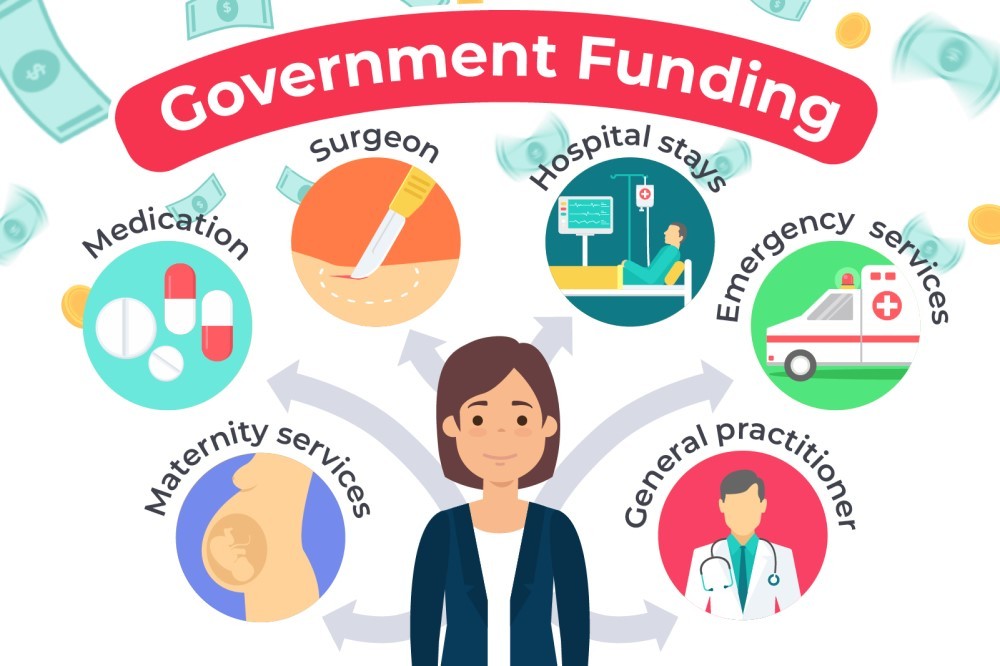
Canada’s publicly funded health care system is dynamic–reforms have been made over the past four decades and will continue in response to changes within medicine and throughout society. The basics, however, remain the same–universal coverage for medically necessary health care services provided on the basis of need, rather than the ability to pay.
How Health Care Services Are Delivered
Canada’s publicly funded health care system is best described as an interlocking set of ten provincial and three territorial health systems. Known to Canadians as “medicare,” the system provides access to a broad range of health services.
What Happens First (Primary Health Care Services)
When Canadians need health care, they most often turn to primary health care services, which are the first point of contact with the health care system. In general, primary health care serves a dual function.
First, it provides direct provision of first-contact health care services. Second, it coordinates patients’ health care services to ensure continuity of care and ease of movement across the health care system when more specialized services are needed (e.g., from specialists or in hospitals).
Primary health care services are increasingly comprehensive, and may include prevention and treatment of common diseases and injuries; basic emergency services; referrals to and coordination with other levels of care, such as hospital and specialist care; primary mental health care; palliative and end-of-life care; health promotion; healthy child development; primary maternity care; and rehabilitation services.
Doctors in private practice are generally paid through fee-for-service schedules that itemize each service and pay a fee to the doctor for each service rendered.
These are negotiated between each provincial and territorial government and the medical professions in their respective jurisdictions. Those in other practice settings, such as clinics, community health centres and group practices, are more likely to be paid through an alternative payment scheme, such as salaries or a blended payment (e.g., fee-for-service payments plus incentives for providing certain services such as the enhanced management of chronic diseases). Nurses and other health professionals are generally paid salaries that are negotiated between their unions and their employers.
When necessary, patients who require further diagnosis or treatment are referred to other health care services, such as diagnostic testing, and health care professionals, such as physician specialists, nurse practitioners, and allied health professionals (health care professionals other than physicians and nurses).
Health Human Resources
In 2006, just over 1,000,000 people in Canada worked directly in health occupations; this represented 6% of the total Canadian workforce.
Health care providers may be regulated (through professional colleges or other bodies) or non-regulated, unionized or non-unionized, employed, self-employed or volunteer.
Most doctors work in independent or group practices, and are not employed by the government. Some work in community health centres, hospital-based group practices, primary health care teams or are affiliated with hospital out-patient departments.
Nurses are primarily employed in acute care institutions (hospitals); however, they also provide community health care, including home care and public health services.
Most dentists work in independent practices; in general, their services are not covered under the publicly funded health care system, except where in-hospital dental surgery is required.
Allied health professionals include: dental hygienists; laboratory and medical technicians; optometrists; pharmacists; physio and occupational therapists; psychologists; speech language pathologists and audiologists.
What Happens Next (Secondary Services)
A patient may be referred for specialized care at a hospital, at a long-term care facility or in the community. The majority of Canadian hospitals are operated by community boards of trustees, voluntary organizations or regional health authorities established by provincial/territorial governments.
Hospitals are generally funded through annual, global budgets that set overall expenditure targets or limits (as opposed to fee-for-service arrangements) negotiated with the provincial and territorial ministries of health, or with a regional health authority or board.
Although global funding continues to be the principal approach for hospital reimbursement in Canada, a number of provinces have been experimenting with supplementary funding approaches.
Secondary health care services may also be provided in the home or community and in institutions (mostly long-term and chronic care).
Referrals to home, community, or institutional care can be made by doctors, hospitals, community agencies, families and patients themselves. Patient needs are assessed by medical professionals, and services are coordinated to provide continuity of care.
Care is provided by a range of formal, informal (often family) and volunteer caregivers.
For the most part, home and continuing care services are not covered by the Canada Health Act; however, all the provinces and territories provide and pay for certain home and continuing care services.
Regulation of these programs varies, as does the range of services. The federal department of Veterans Affairs Canada provides home care services to certain veterans when such services are not available through their province or territory.
In addition, the federal government provides home care services to First Nations people living on reserves and to Inuit in certain communities.
In general, health care services provided in long-term care facilities are paid for by the provincial and territorial governments, while room and board costs are paid for by the individual. In some cases, payments for room and board are subsidized by the provincial and territorial governments.
Palliative care is delivered in a variety of settings, such as hospitals or long-term care facilities, hospices, in the community and at home.
Palliative care focuses on those nearing death and their families and includes medical and emotional support, pain and symptom management, help with community services and programs, and bereavement counselling.
Additional (Supplementary) Services
The provinces and territories provide coverage to certain people (e.g., seniors, children and low-income residents) for health services that are not generally covered under the publicly funded health care system.
These supplementary health benefits often include prescription drugs outside hospitals, dental care, vision care, medical equipment and appliances (prostheses, wheelchairs, etc.), and the services of other health professionals such as physiotherapists. The level of coverage varies across the country.
As noted earlier, those who do not qualify for supplementary benefits under government plans pay for these services through out-of-pocket payments or through private health insurance plans.
Many Canadians, either through their employers or on their own, are covered by private health insurance and the level of coverage provided varies according to the plan purchased.
Trends/Changes in Health Care
The Canadian health care system has faced challenges in recent years due to a number of factors, including changes in the way services are delivered, fiscal constraints, the aging of the baby boom generation and the high cost of new technology.
These factors are expected to continue in the future.
Since publicly funded health care began in Canada, health care services and the way they are delivered have changed–from a reliance on hospitals and doctors to alternative care delivery in clinics, primary health care centres, community health centres and home care; treatment using medical equipment and drugs; and a greater emphasis on public health and health promotion.
Medical advances have led to more procedures being done on an out-patient basis, and to a rise in the number of day surgeries. Over the past several decades, the number of nights Canadians spent in acute-care hospitals on a per capita basis has declined, while post-acute and alternative services provided in the home and community have grown.
Beginning in the mid-1990s, most provinces and territories worked to control costs and improve delivery by decentralizing decision-making on health care delivery to the regional or local board level. Such regional health authorities are managed by appointed members who oversee hospitals, long-term care facilities, home care and public health services in their area. However, in recent years, some provinces have moved away from a decentralized model of health care delivery in favour of consolidating the number of health authorities and centralizing decision-making structures.
Primary Care
The episodic and responsive traditional primary health care model has served Canadians well.
However, the aging population, rising rates of chronic disease, and other changing health trends have emphasized the need for the health care system to maintain and continue to develop the capacity to respond to the changing needs of Canadians.
Reforms have focused on primary health care delivery, including setting up more community primary health care centres that provide on-call services around-the-clock; creating primary health care teams; placing greater emphasis on promoting health, preventing illness and injury, and managing chronic diseases; increasing coordination and integration of comprehensive health services; and improving the work environments of primary health care providers.
eHealth
Advancing eHealth has been a focus of attention in Canada and several other countries.
Electronic health technologies (such as electronic health records and telehealth) are significant drivers of innovation, sustainability and efficiency in the health care system by improving access to services, patient safety, quality of care, and productivity.
The implementation and use of electronic health records contributes to primary health care renewal by facilitating the effective coordination and integration of services amongst care providers.
Wait Times Reduction
Provincial and territorial efforts to reduce acute care wait times in accordance with the priorities of their individual systems include: training and hiring more health professionals; clearing backlogs of patients requiring treatment; building capacity for regional centres of excellence; expanding ambulatory and community care programs; and developing and implementing tools to better manage wait times.
Patient Safety
Patient safety, including the avoidance of medical errors or adverse events, is one of the most significant issues facing health systems globally, and is a growing aspect of Canada’s efforts to improve the quality of health care provided across the health care system.
The federal, provincial and territorial governments are continuing to work with health care professionals, organizations and institutions to better understand and mitigate the risks involved in the delivery of health care. This includes the development and implementation of a range of measures to improve patient safety and the quality of care.
Canada's health system is free